Dental payers and providers have the same mission: to help people receive the dental care they need.
But dental insurance is complex, and legacy processes can lead to payer-provider friction and impact member care.
Now Overjet’s artificial intelligence (AI) technology is helping to streamline processes, review claims and pre-authorization requests faster, and strengthen the payer-provider relationship through an end-to-end utilization review management system.
What Dentists Want from Insurance Companies
When dentists submit a claim for patient care, they want to:
- Have submissions paid quickly
- Reduce the back-and-forth of requests for additional information
- Understand the insurer’s guidelines for medical necessity
- Have greater transparency into why a claim may be denied
- Provide the best outcome for patients
What Dental Payers want in their Utilization Review Process
Dental payers want an efficient utilization review process to:
- Ensure claims meet medical necessity guidelines
- Reduce the back-and-forth of requests for additional information
- Streamline processes
- Drive affordability in the plan products
- Provide the best outcome for members
AI Redefines the Dental Healthcare Journey
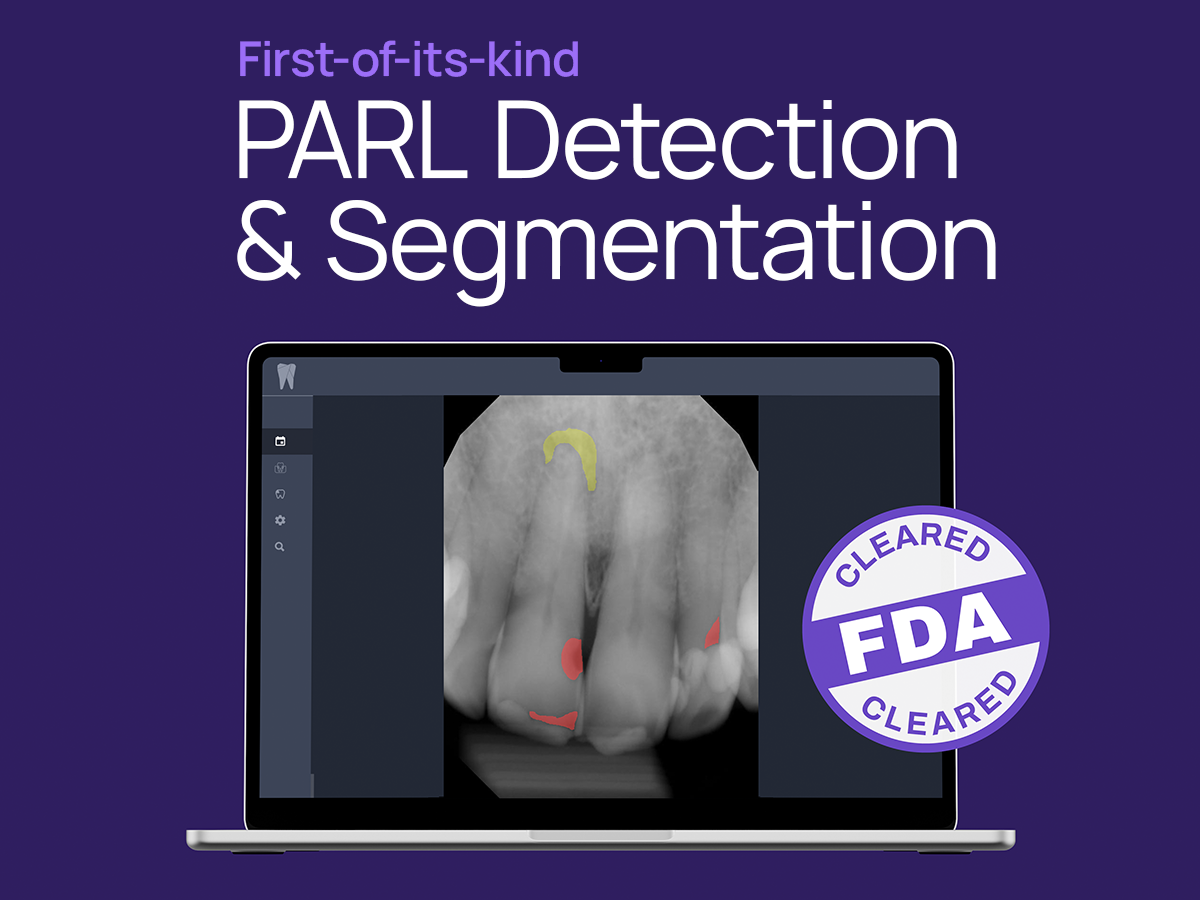
 Dentists are integrating AI-powered radiograph analysis and clinical insights into their daily workflow. Overjet’s technology helps dentists detect cavities and calculus, and it quantifies bone level measurements, which dentists use to help diagnose periodontal (gum) disease. Overjet also analyzes patient records from previous visits to help identify potential treatment needs.
Dentists are integrating AI-powered radiograph analysis and clinical insights into their daily workflow. Overjet’s technology helps dentists detect cavities and calculus, and it quantifies bone level measurements, which dentists use to help diagnose periodontal (gum) disease. Overjet also analyzes patient records from previous visits to help identify potential treatment needs.
Overjet’s AI not only helps dentists in their clinical decision-making, but is a powerful patient communication tool. When patients see their X-rays with the AI findings, they better understand the treatment their dentist is recommending.
On the payer side, AI-driven utilization review and claims management optimizes the entire process. Here’s how it works with Overjet’s AI technology:
Claim Submitted: The dental practice submits claims the same way as always. Typically, Overjet’s AI technology can process even low-quality, non-digital images.
Claim Analyzed: Overjet analyzes the submissions of over 350+ procedure codes to see if they meet the medical necessity guidelines established by the payer. Overjet’s AI can analyze clinical evidence beyond just radiographs to include intra-oral photographs and narratives.
Claim Recommendation: If the claim meets the medical criteria, it’s automatically approved. If the claim is missing information, then an automated request can be sent back to the provider. If the claim does not automatically meet the medical necessity guidelines, Overjet’s Augmented Workflow solution immediately routes the claim to the payer’s clinical review staff or to Overjet’s dental consulting service for further evaluation.
By consolidating all reviewers and data into one platform, Overjet simplifies the process while improving consistency and efficiency.
The Benefits of AI-Powered Utilization Review in Dental
Overjet’s Claim Intelligence platform simplifies utilization review and enables consistency, efficiency, and a better experience for providers, payers, and patients.
- 80% increase in consistency of review. AI helps remove the guesswork from dental work by applying the medical necessity guidelines objectively and consistently every time.
- 80% reduction in manual review. The AI helps payers manage claims in one simplified platform, and significantly reduces the need for administrative reviews.
- 80% faster claim reviews. With the AI analyzing and annotating the submissions, it provides the clinical reviewers with more data to help them with their clinical decision-making. Typically, it reduces the amount of time it takes to review a claim from 5 minutes to 1 minute.
Alleviating Friction Between Payers and Providers
By providing transparent, evidence-based criteria to assist in determining medical necessity, AI alleviates many of the points of friction.
Not only does it help ensure objectivity in claim decisions, but the automation reduces delays in requests for missing claim documentation. The AI analysis improves the speed of both pre-authorization requests and claim reviews. And that’s just the beginning.
In the near future, point-of-care adjudication may be possible. For dentists, this means they can submit their diagnosis and treatment plan to the payer while the patient is still in the chair, and receive a benefit decision within minutes. That will alleviate one of the biggest challenges for patients: knowing whether insurance will cover the cost of their care.
Resources:
To learn more about how Overjet can help payers modernize their utilization review process with AI, visit Overjet.ai.
Please click here to watch the NADP webinar on Strengthening the Payer-Provider Connection: Leveraging the Power of AI to Improve Oral Health. It’s free to create an NADP account and free to view.